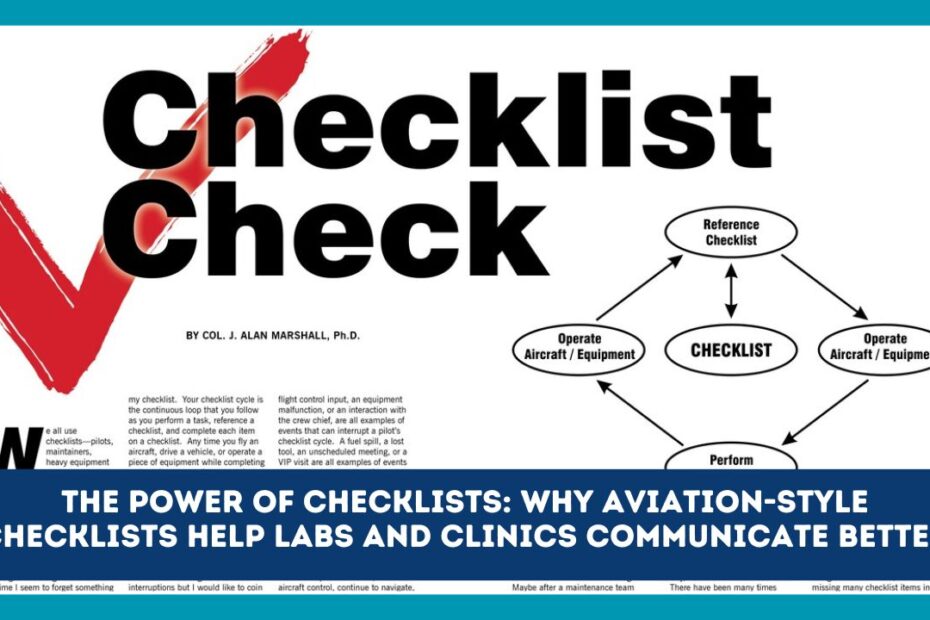
In aviation, checklists are treated like safety equipment. They turn complex routines into simple, reliable steps—especially when people are busy, tired, or stressed. Labs and clinics face the same pressures: time-critical work, handovers, instruments with quirks, and decisions that affect patient safety. Bringing aviation-style checklists into healthcare is a low-cost way to cut errors, speed up teamwork, and make communication crystal clear.
Why communication breaks down in labs and clinics
Even skilled teams miss things when:
- Workloads spike and cognitive load is high
- Staff rotate across shifts and locations
- People rely on memory or informal habits
- Background noise and interruptions break focus
- There’s no shared mental model for who says what, when
Checklists don’t replace expertise; they support it. They create a shared sequence, common language, and clear pause points where the team slows down just long enough to confirm the right next step.
What makes aviation-style checklists different
A good aviation checklist is not a policy document. It’s a short, action-oriented tool designed for the moment of use.
Core features:
- Phase-based: before, during, after (e.g., before collection, during analysis, post-result).
- Challenge–response: one person calls the step (“Patient ID?”), another confirms (“Two identifiers matched.”).
- Read-do or do-confirm: either read each step then do it, or do the routine and confirm critical items at the end.
- Plain language & verbs: “Label tube” beats “Ensure proper labeling.”
- Built-in communication checks: call-outs (“Critical potassium 6.8”) and read-backs (“Confirming six-point-eight”).
- Role clarity: a named checklist leader guides the flow, others respond.
Where checklists help most in healthcare
- Specimen collection & labeling (mislabeling is a tiny mistake with huge consequences)
- Instrument startup/shutdown and maintenance
- Pre-analytical acceptance (sample integrity, transport time, temperature)
- Result verification & release (delta checks, reflex testing)
- Critical result communication (who to call, what to say, read-back)
- Shift handovers (reduce “I thought you did it”)
- Emergency response (spills, exposure, code situations)
Anatomy of a high-impact checklist
Keep it short and visible. Aim for 5–9 items per section.
- Trigger: When to use it (“Before any blood draw”).
- Roles: Who leads; who responds.
- Steps with verbs: One line each, minimal words.
- Pause points: Small stops to confirm the critical few.
- Verification style: Read-do vs do-confirm.
- Time/initials: Space to sign or tick—creates accountability.
- Version date: So staff know it’s current.
Ready-to-use sample checklists
1) “Before Specimen Collection” (Read-Do)
Leader: Collector Responder: Assistant (or self-confirm if alone)
- Patient identity: Two identifiers matched with wristband and order.
- Order verified: Test, priority, and site confirmed in LIS.
- Allergies/precautions: Anticoagulants, latex, infection status checked.
- Tubes & labels ready: Barcodes printed; labels match patient & test.
- Site prepped: Correct patient, correct limb/site, clean & dry.
- Time stamp: Collection time recorded on requisition/LIS.
- Label at bedside: Label applied in presence of patient.
- Specimen integrity: Invert as required; temperature/ice if needed.
- Handover: Transport logged; chain of custody if applicable.
Pause point: “Team agrees to proceed?” → Yes.
2) “Critical Result Call & Read-Back” (Challenge–Response)
Leader: Caller (lab) Responder: Receiver (clinician/ward)
- Identify yourself & lab (name, department).
- Confirm receiver (name, role, patient location).
- Patient identity (two identifiers).
- State critical result (call-out exact value and units).
- Receiver read-back (word-for-word result and units).
- Action window (is action time-sensitive? yes/no).
- Next step & responsibility (who does what, by when).
- Document call time, names, read-back success in LIS.
- Escalation if no answer or disagreement (define levels & timing).
Pause point: “Do we both confirm the same value and plan?” → Yes.
3) “Shift Handover: SBAR Mini-Checklist” (Do-Confirm)
S – Situation: Today’s status, pending runs, out-of-service equipment.
B – Background: Relevant patient or batch notes; QC trends.
A – Assessment: Risks (stock low, instrument drift, staffing gaps).
R – Recommendation: Next actions, who is responsible, deadlines.
Tick when done: ☐ LIS notes updated ☐ Whiteboard updated ☐ Keys/cards transferred
4) “Instrument Startup (Analyzer X)” (Read-Do)
- Power on; self-test complete (no major faults).
- Reagents within expiry; onboard volumes above thresholds.
- QC levels loaded; lot numbers match LIS.
- Run daily QC; review flags; document corrective actions.
- Temperature/pressure within limits; print or save auto-log.
- Maintenance tasks done (waste emptied, probes cleaned).
- Status set to “Ready” in LIS; notify bench lead.
How to roll out checklists without resistance
- Co-design with users: Techs, nurses, phlebotomists, residents. Ask, “Where do mistakes hide?”
- Start small: Pilot in one workflow (e.g., blood culture collection).
- Run short simulations: Practice the call-and-response rhythm.
- Make them easy to find: Laminated copies at workstations + quick links in the LIS/EHR.
- Name a checklist leader: On each shift, someone owns updates and answers questions.
- Audit lightly, learn weekly: Track near-misses, mislabels, turnaround times, and communication delays. Share wins quickly.
- Keep it living: Trim steps that add no value; bold the critical few; review quarterly.
Measuring impact (simple scorecard)
- Specimen mislabel rate ↓
- Critical result notification time (collection → clinician informed) ↓
- Turnaround time outliers ↓
- QC/maintenance misses ↓
- Staff confidence & onboarding speed ↑
- Incident reports tied to communication breakdowns ↓
Even two or three of these moving in the right direction can justify the effort.
Common pitfalls (and fixes)
- Too long: If it doesn’t fit on one page or one screen, it won’t be used. Fix: Split by phase.
- Vague wording: “Ensure” and “appropriate” invite confusion. Fix: Use clear verbs and measurable checks.
- No trigger: People forget when to use it. Fix: Put trigger in the title (“Before Result Release”).
- No owner: Checklists decay without stewardship. Fix: Assign an owner per area with a review cadence.
- Punitive rollout: Staff hide mistakes if tools feel like surveillance. Fix: Frame as safety support, not policing.
Quick template you can copy
TITLE (Trigger): e.g., “Before Specimen Collection”
ROLE: Leader ______ Responder ______ VERSION: ______ DATE: ______
[ ] Step 1 (verb + object, measurable)
[ ] Step 2
[ ] Step 3
PAUSE POINT: Team confirms _______________
NOTES (limits, units, ranges):
ESCALATION: Who to call if blocked: ____________________
SIGN/OFFICIAL: _________ TIME: ________
Conclusion
Aviation-style checklists help labs and clinics do the right things, in the right order, at the right time—together. By building short, clear lists with challenge–response, read-backs, and defined pause points, you turn individual know-how into team reliability. Start with one high-risk task, co-design with the people who use it, and track a few simple metrics. In a matter of weeks, you’ll see fewer miscommunications, faster handovers, and safer care—without adding cost or complexity.